Module 3: Epidemiology using COVID-19
Modeling Infectious Diseases
Epidemic Curve
An epidemic curve, or epi curve, is a graphical display of the number of illnesses caused by a disease outbreak over time.
Exercise 2
Exercise
Complete the CDC’s training on Epidemic Curves, here.
Predict. What do you predict would be the shape of the epi curve of the COVID-19 illness in a community? Draw your prediction and label your figure.
Solution
An example of an epi curve
SIR Model
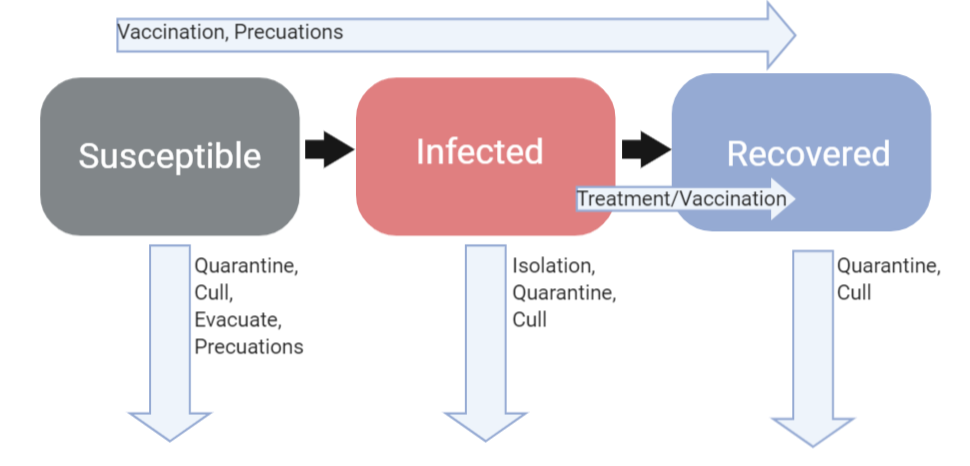
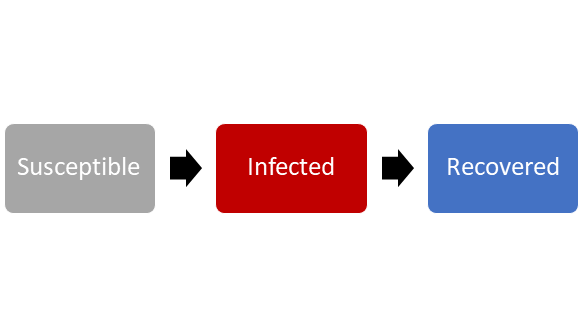
Epidemiologists and disease ecologists use models to help predict the spread of infectious diseases throughout a community or ecosystem. Using a SER Model, individuals are classified according to their disease status into the following categories:
- Susceptible: Individuals in this category are susceptible to infection by the parasite. These individuals have not previously been in contact with the parasite, nor do they have any immunity to the parasite.
- Infected: Individuals in this category have been exposed to and infected by the parasite. These individuals may be infectious, and are capable of spreading the parasite to others. Infectious individuals will often display symptoms of the illness caused by the parasite. However, some individuals may not display any symptoms, but are still capable of spreading the parasite. These individuals are asymptomatic carriers of the infection.
- Recovered: Individuals in this compartment are no longer infectious. Once the parasite is detected by the host’s immune system, the immune system fights off the infection. Individuals that recover from infection have often acquired immunity to the parasite.
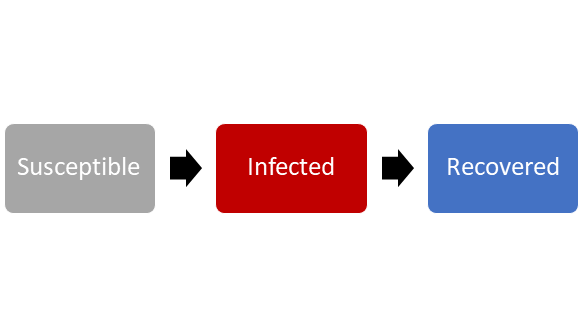
Foundations of the SIR Compartmental Model. The flow between these compartments is affected by many different factors that include an individual’s health, public health, and environmental conditions.
Question 1
Question
When does an individual move between the three categories? What determines the rate of this movement?
Solution
An individual remains in the susceptible category until they are (1) exposed to the parasite and (2) infected by the parasite. The probability of exposure to the parasite and the probability of infection by the parasite will determine how quickly individuals in the S category move into the I category.
An individual remains in the infected category for the length of time that an individual is capable of transmitting the infection to susceptible individuals. This is known as the infectious period.
An individual moves from the infected category into the recovered category once the host’s immune system clears the infection.
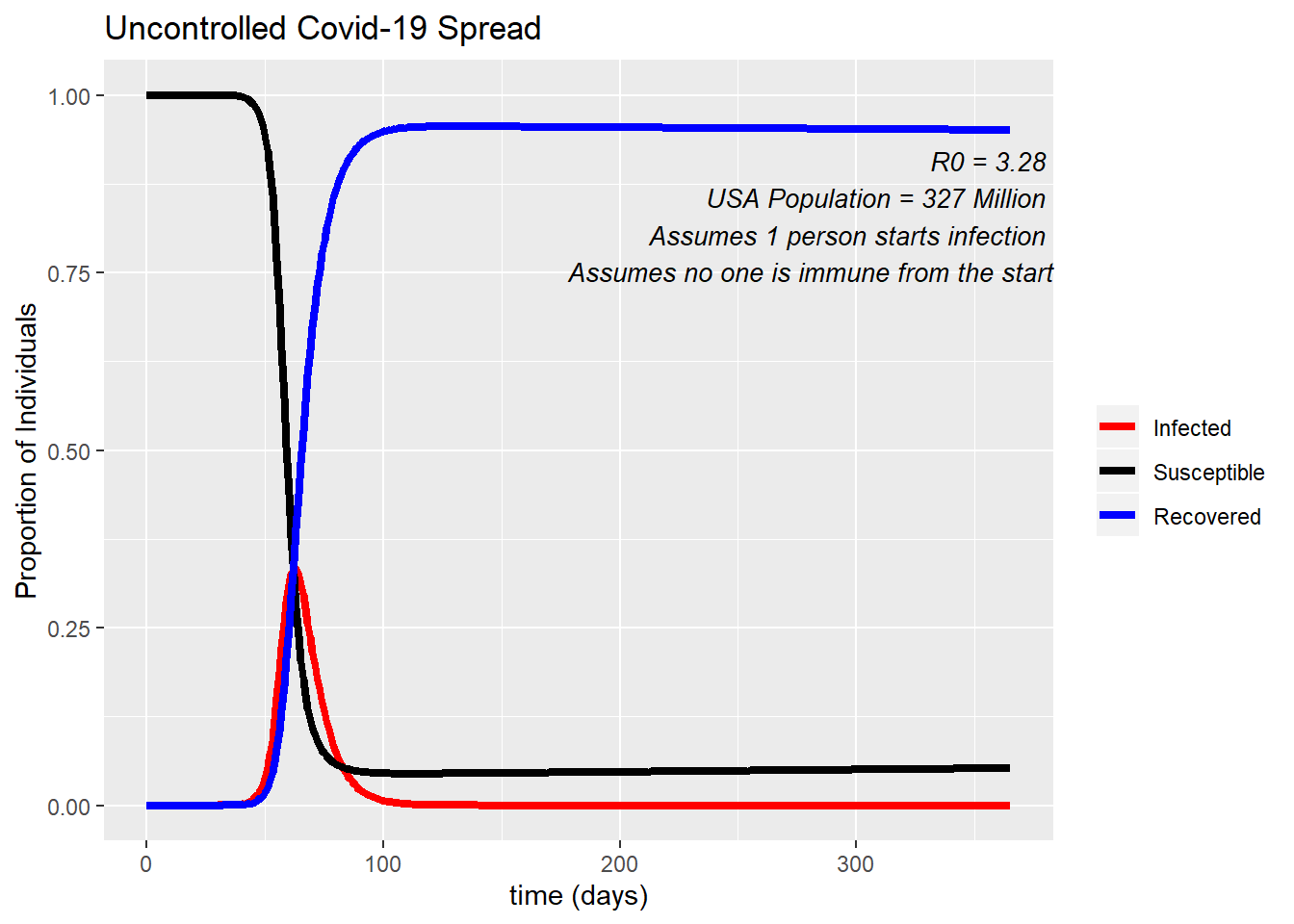
SIR Model and the Whole Population
The same principles that apply to an individual moving between compartments in the SIR model can be applied to a whole population. The graph below is an example of how an SIR model can be applied to the United States population for COVID-19. In this example we start with only one person entering the US who is infected with COVID-19, and how quickly this can spread if left totally uncontrolled. After 100 days almost the entire population of the US (all 327 million) have been infected - the only ones left in the Susceptible compartment are those being born, and immigrating in. At the peak of infection 35% of Americans would be sick at a single time, which is 114,450,000 people!
Question 2
Question
Under what conditions does the number of infected individuals increase and decrease?
Solution
The number of infected individuals will increase if more individuals enter this category than leave this category. That is, more individuals are becoming infected than reaching recovery. The number of infected individuals will decrease when more individuals are recovering than getting infected, usually because the pool of susceptible individuals has decreased.
Speed of Spread
How fast can an infection spread through a community?
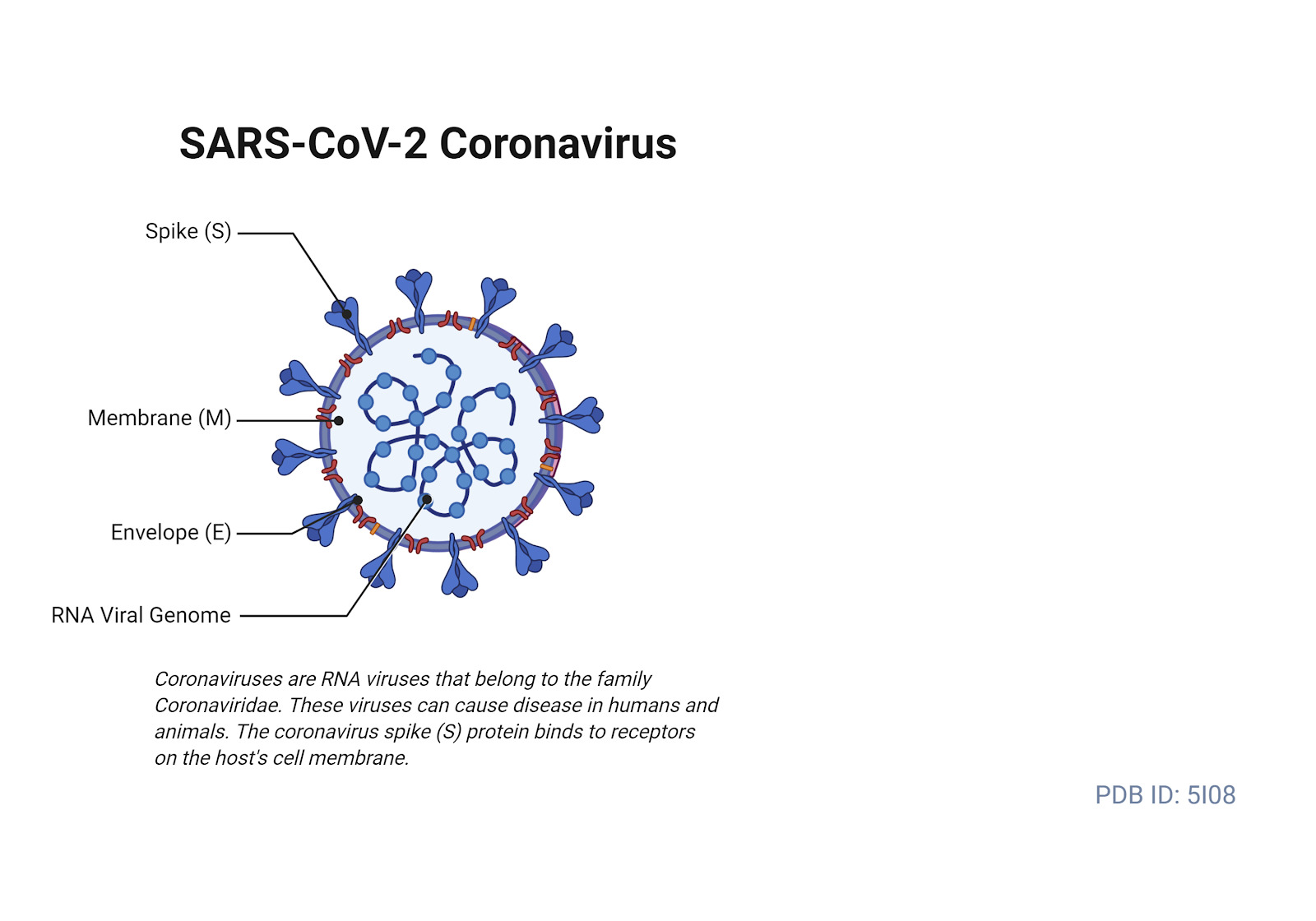
The speed at which a parasite can spread through a community is related to the basic reproductive number of the pathogen, the R0 value. You may have noticed it on the “Uncontrolled COVID-19 Spread” graph.
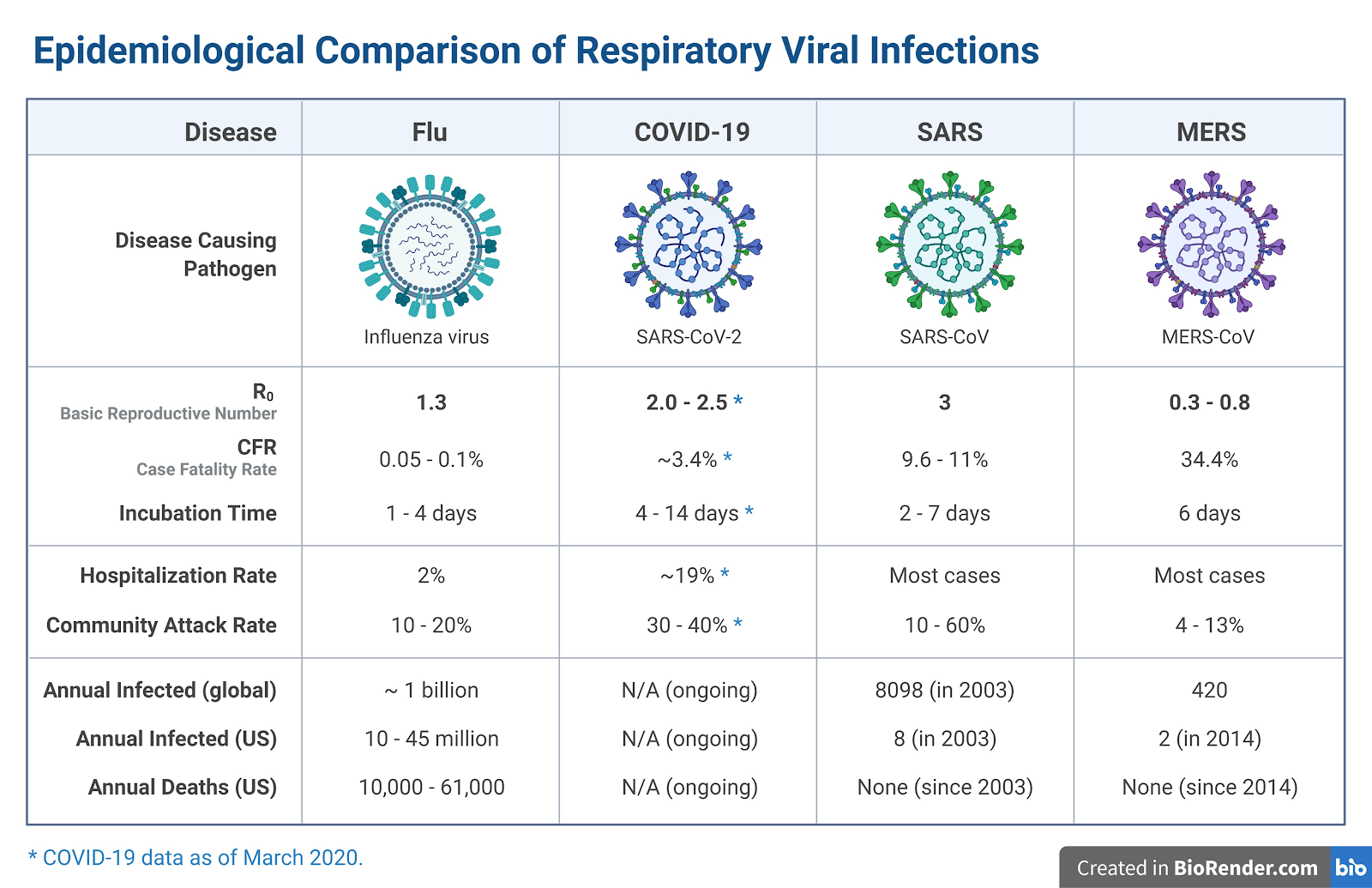
The R0 value is the number of new infections caused by a single infected individual. The R0 of the COVID-19 infection has been found to have a range from 1.4 - 6.49, with an average of 3.28.(The scientific article that found this can be located here). This range is due to time period, location, and method of calculation. This means, on average, for every infected individual, there are expected to be 3 new cases that arise.
Exercise 3
Exercise
Model the spread of the COVID-19, beginning with a single infected individual and assuming an R0 of 2. How many infections may arise after five generations? The first two generations have been modeled for you. 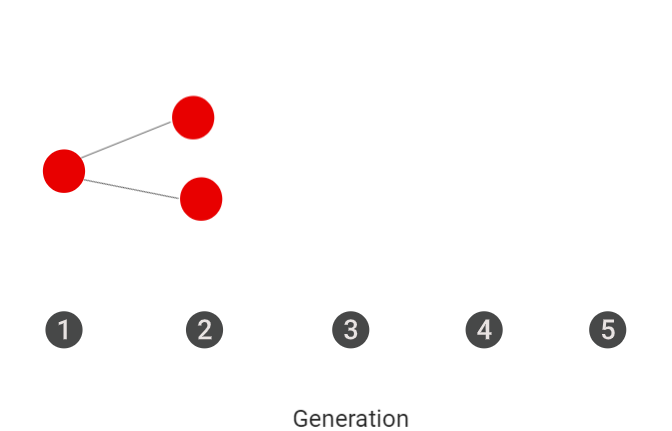
Solution
In the 5th generation there should be 16 infected individuals in the 5th generation.
Exercise 4
Exercise
Make a prediction. Order the following diseases by their contagiousness (R0): COVID-19, Influenza, Measles, Bubonic Plague. Use the MicrobeScope Application to compare R0 of different diseases.
Solution
R0 influenza = 1.53
R0 measles = 12-18
COVID-19 = 3.28
Plague = 3.5
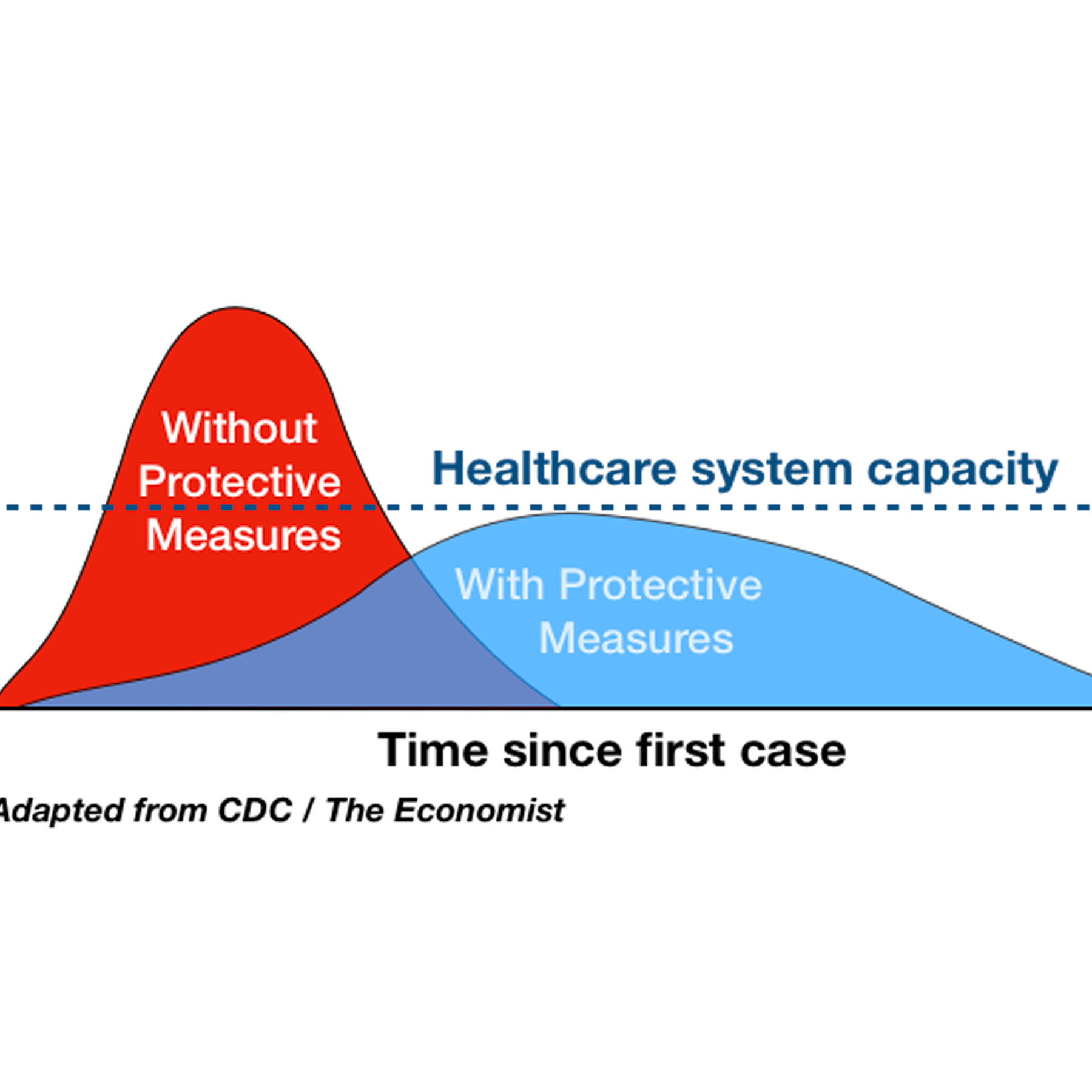
Public Health Measures
There are multiple public health measures that can be put into effect with the aim of stopping or limiting the spread of an infectious disease in a population. Which measure is implemented is typically determined by disease itself, and what population it is infecting. There are six different measures that can be used on their own or in collaboration with each other. The most effective responses to slow the spread of an epidemic typically involve more than one public health measure.
Isolation
Isolation is when you remove infected persons from the population. This limits or completely stops their contact with those in the susceptible population, slowing the spread of disease in the population.
Quarantine
The term quarantine refers to the 40 day period that people had to remain on ships before coming to land during the time of the Plague. Now when people quarantine it refers to them removing themselves from the population before or after exposure to the disease. Doing so protects themselves from possibly acquiring the infection, if they end up being infected it is also protecting the population from acquiring it from them.
In the United States, many cities, counties, and states are issuing mandatory “Stay-At-Home” or “Safer-At-Home” orders to their citizens. These orders are telling people to remain in their home and asking them only to leave for essential functions (e.g. essential jobs, grocery shopping, doctor’s visits). This is a type of quarantine, and when people participate properly they are playing their part in slowing the spread of COVID-19. In the graph below, you can see how the proportion of people infected changes based on what percent of the population abides by the “Safer-At-Home” orders. 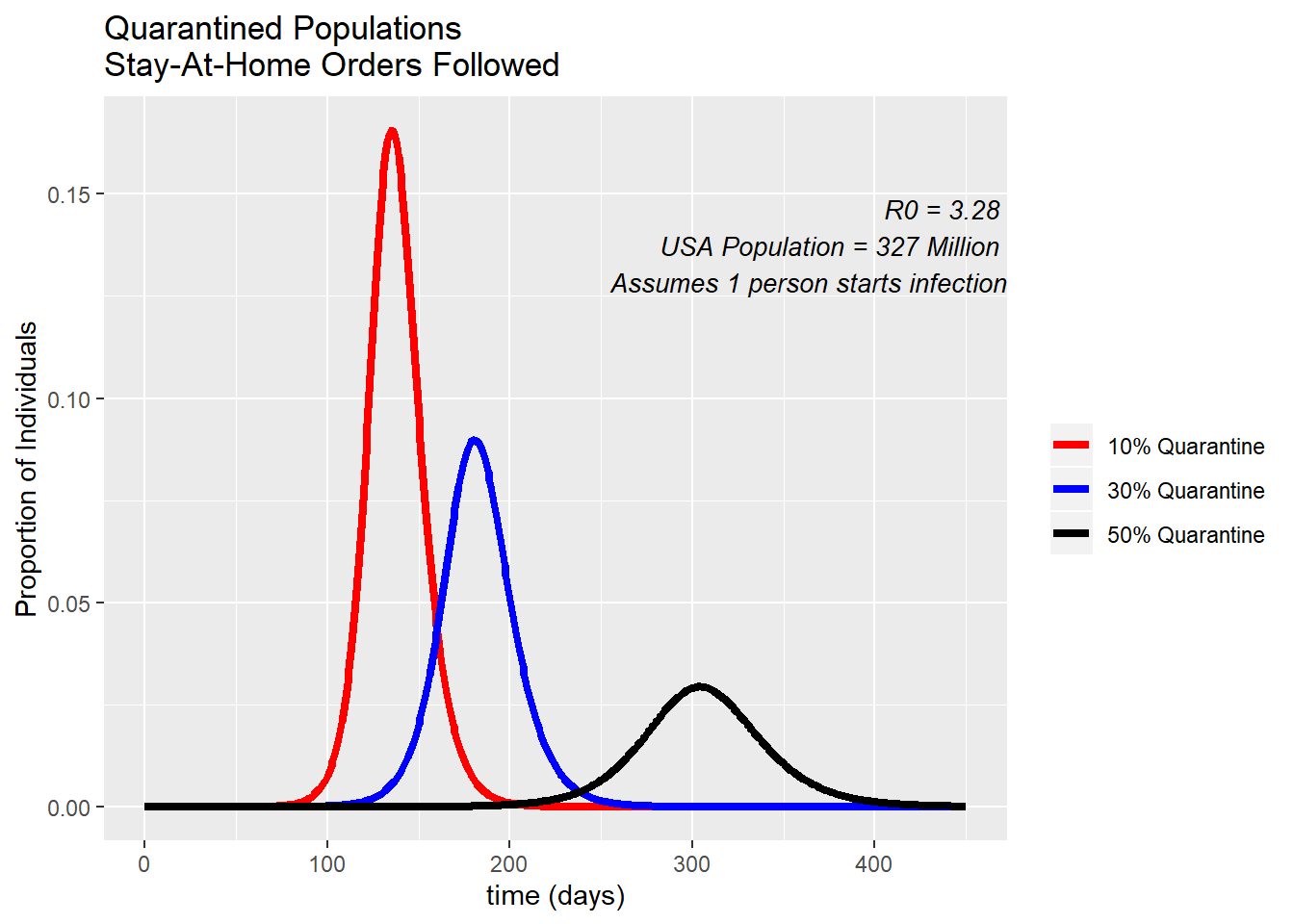
The percent of people participating in the quarantine are based on a recent study by Unacast. If you take a look at this website, you can see how US states are scoring in lowering their activity and social distancing. Wyoming is doing the worst by only decreasing their activity by 10%, while some states have decreased their activity by 50%. In the United States as a whole, we have decreased our activity by about 36%.
Treatment (vaccine/drugs)
Many diseases have preventative vaccines, or effective drugs that can be used to decrease the spread of the disease. Having a vaccine can make people “recovered” from the disease without ever having to be infected. Drugs that are used for treatment will be targeting those in the infected category, decreasing their infectious period. However, developing these treatments is not an easy feat. Treatments and vaccines for COVID-19 are still in development, some have made their way into clinical trials but it can still take months to be approved by the FDA for general use even on a fast track program.
Evacuate
Evacuation is implemented by removing susceptible individuals from the population. In public health this is typically used during times of natural disasters. However, evacuating a population can also play a role in how a disease will spread. For example, the population of a state being evacuated while it’s on the path of a category 5 hurricane. The more people that stay in the path of destruction get put at higher risk of being exposed to and being infected by a disease.
Take Precautions (face masks)
Precautions are also being pushed by public health officials during the COVID-19 pandemic. Precautions include washing your hands properly, using gloves and face masks, respiratory hygiene, cough etiquette (covering your coughs and sneezes), and cleaning and disinfecting environmental surfaces. Doing any or all of these precaution measures can decrease your risk of contracting the disease, and can lower the risk of the passing on the disease.
Culling
Culling is the act of decreasing the population through selective slaughter. This is not a measure used on humans for human disease, it is most often used in cattle and some wildlife diseases. In diseases that are passed directly from animals to humans, when an outbreak of that disease is occurring one of the measures quickly implemented is the culling of the population of infected animals.
Exercise 5
Exercise
Using the SIR compartmental model and the 6 public health measures above, draw arrows describing how each measure will affect the population. Label the arrows with the measure. Note: some measures can affect more than one compartment.
Solution